Healthy gut, Happy mind
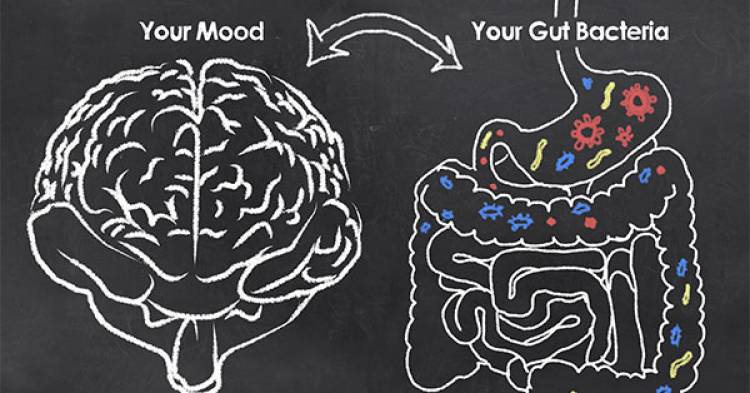
Did you know that serotonin, the body’s own personal happy-drug, is produced mainly in the gut? What about the fact gut bacteria help produce neurotransmitters that help us feel calm? And that the gut is sometimes called our ‘second brain’?
The more we learn about gut bacteria, the more we understand how closely these bacteria work with our brains. So, could it be true that a healthy gut can make us happy?
A gut feeling
The English language is littered with references linking our gut with our emotions. Think about it. Have you heard someone say, ‘it’s a gut feeling’ or ‘I can feel it in my guts’? Maybe you’re feeling nervous so you say: ‘I’ve got butterflies in my tummy.’ Once upon a time, centuries ago, you’d say to someone ‘I love you with all my bowels’ rather than ‘I love you with all my heart’. We knew back then that emotions and mood were linked with our digestive system. It’s only recently we’re learning why.
Gut-brain talk
The digestive system is linked to the brain by a series of nerve pathways. This link is called the gut-brain axis and it helps the brain coordinate and check digestive functions. It also connects the emotional and thought areas of the brain with functions of the gut, including control of the immune system and hormone production. Communication goes both ways, from brain to gut and gut to brain.
If you’re feeling depressed, another system of the body is affected. Called the hypothalamic-pituitary-adrenal (HPA) axis, this controls the body’s reaction to stress. When depression is resolved, the HPA goes back to functioning normally. In 2004, research on mice bred in a germ-free environment showed that bacteria are crucial for the HPA to work normally, therefore reducing stress reactions.
Other research on mice has shown their microbiota (gut bacteria, fungi, archaea and viruses) doesn’t just influence stress, but stress influences the microbiota. One study found infant mice separated from their mothers grew different bacteria to those who didn’t have the stress of being separated from their mothers. So, it seems our gut bacteria are involved in a two-way conversation with our body.
While we don’t have such clear experiments with human subjects, we do know that people with depression tend to have very different microbiota to those that don’t have depression. People with depression tend to grow more bacteria from the Firmicutes, Actinobacteria and Bacteriodetes groups and fewer from the Bifidobacteria and Lactobacillus groups, as well as having a wider diversity of microbiota in the gut. Taking the bacteria from chronically depressed people and putting them into rats who were lacking their own bacteria led to the rats taking on the behaviours and body system changes seen in people who were chronically depressed.
Move over probiotics, psychobiotics are the new superhero
What we’re now learning is that gut bacteria have an important role in the two-way
communication between our brain and our gut. This role is thought to be so important, the next wave of anti-depression medications is being designed to help symptoms by modifying gut bacteria. They’ve even coined the term ‘psychobiotics’ for this, as supplementing with certain probiotics may significantly reduce anxiety and depression scores.
As people with depression and anxiety seem to grow fewer Lactobacillus and Bifidobacterium species, this is where a lot of the probiotic supplement research has focused. But more than that, these genera don’t cause inflammation like other bacteria may do – and inflammation is a key feature of gut damage.
How a high-fat western-style diet can make you depressed (but a Mediterranean-style diet won’t)
A Western-style diet, high in saturated fats, sugars and refined or processed foods, has been shown to alter the gut microbiota in a similar pattern to growth we find in people with depression. The result of this change in bacteria with the high-fat Western-style diet is a more permeable gut lining and greater risk of anxiety and depression.
However, the opposite growth pattern of bacteria is what we find if you eat a Mediterranean-style diet high in legumes, nuts, vegetables, fruit, extra virgin olive oil and whole grains with moderate intake of fish and chicken and only a little red meat.
The three Ps…
Prebiotics
are undigested carbohydrates used by our gut bacteria as food.
Probiotics
are ‘friendly’ bacteria used to promote gut health.
Psychobiotics
are probiotics and prebiotics that may help with mental health by altering gut bacteria.
Food and activities that promote gut health for better mood
Taking care of what you eat can help you grow great gut bacteria. In turn, managing stress can also support your healthy gut bacteria.
1. Reduce how much processed (high saturated fat, salt and sugar) food you eat.
2. Follow a Mediterranean diet style, focusing on prebiotic foods such as:
- plenty of fresh, seasonal
- vegetables and fruit
- legumes, pulses, nuts and seeds
- wholegrain products
- mainly plant-based meals, with chicken or fish and only a little red meat
- extra virgin olive oil.
3. Consider taking a probiotic.
4. Participate in mindful exercise.
5. Try to manage your stress as much as you can.
What to look for in a probiotic for mood?
Walk into a pharmacy and you’ll come face to face with shelves of probiotics. Each has a different mix of bacteria and yeasts. So which ones may help with depression or anxiety?
Research on human subjects suggests the following bacteria may help with your mood. These can be safely taken alongside any other medications you may be taking for that reason:
- Lactobacillus helveticus and Bifid bacterium longum together may lead to a reduction in measures of anxiety and depression
- Lactobacillus casei Shirota, found in Yakult, may improve mood in those with low mood, or anxiety in those with chronic fatigue syndrome
- Lactobacillus acidophilus, Lactobacillus casei and Bifidobacterium bifidum may reduce depression index scores
- Lactobacillus gasseri and B. longum together may reduce ACTH (a hormone produced during stress) but not depression
- L. casei, L. acidophilus, L. rhamnosus, and L. bulgaris; Bifidobacterium breve and B. longum; and Streptococcus thermophilus (fermented yoghurt) may reduce anxiety and depression
- B. longum may reduce depression but not necessarily anxiety.